Vasectomy Reversal
Description of Procedure
Sperm are produced in the seminiferous tubules of the testis. This process which takes about 2 months. Next, the sperm flow into the epididymal tubules where they continue to mature. This takes about 2-3 weeks. It is not until the sperm exit the epididymal tubules that they are mature enough to fertilize an egg. The vas deferens is the tube which carries sperm from the epididymis to the prostatic urethra. It is in the urethra where the other components of the ejaculate (prostate and seminal vesical secretions) are mixed and then expelled during ejaculation. Sperm only constitute about 10% of the ejaculatory volume - this is the reason that men will not be able to perceive any change in the ejaculate following a vasectomy.
Obstruction of the vas deferens does not stop sperm production. Sperm continue to be produced but are re-absorbed by the body. Some parts of the sperm are not easily digestible and therefore parts of sperm accumulate within the tubules 'upstream' of the vasectomy site (towards the testis). This can clog the tubules. This 'sludge' can propegate up from the vas deferens into the epididymis preventing the free flow of sperm even once the vas deferens is re-connected. This is a major reason for technical failure of vasectomy reversal.
Sperm can be surgically retrieved from the testis (TESE) or epididymis (PESA) and can be used to achieve a pregnancy when combined with IVF.
Sperm from the testis and epididymis are immature and usually retrieved in low concentrations. As a result, surgically retrieved sperm (via TESE/PESA) require IVF (usually in combination with ICSI) to obtain a pregnancy. Surgically retrieved sperm are almost never satisfactory for insemination (IUI).
What is a Vasectomy Reversal?
Vasectomy reversal (VR) is one method to obtain a pregnancy when the vas deferens has a focal obstruction - most commonly when the vas has been divided intentionally at vasectomy or by inadvertent injury to the vas deferens (for example, with scrotal surgery). The testis continues to produce sperm following obstruction and the goal of VR is to restore continuity to the male reproductive tract so that sperm can once again enter the ejaculate. There are instances of vasal obstruction where VR is not feasible - for extensive or long injuries to the vas, when the vas deferens is obstructed downstream of the inguinal ring (in the pelvis) or when there is an upstream issue (for example, within the epididymis).
In those for whom VR is feasible, it can allow a couple a method to conceive natrually. Furthermore, technically successful VR can result in satisfactory numbers of sperm that can be used with assisted reproduction (ideally insemination/IUI but also IVF and ICSI) if natural conception fails - without the additional need for surgical sperm retrieval. There are many reasons why men pursue reversal, such as the loss of a child or new relationships.
Vasectomy Reversal vs. Alternatives (Sperm Retrieval + IVF)
While vasectomy reversal is often successful, there are other options for having children in the setting of prior vasectomy. Most couples considering vasectomy reversal should also consider a combined approach of surgical sperm retrieval (TESE or PESA) in combination with IVF. Unfortunately, surgically retrieved sperm cannot be used for insemination (intraurterine insemination is one of the least expensive forms of assisted reproduction). For completeness sake, adoption and donor insemination are also options.
Which approach makes the best sense for a couple ultimately comes down to the risks and benefits of each approach. Considerations should include:
Chance of success - most importantly defined as pregnancy and delivery of a healthy baby
Time considerations - how quickly the intervention can occur and the speed with which success or failure can be declared
Options for salvage if the chosen procedure fails
Health risks and treatment burden and the distribution those risks to the man or woman
Expense
For many couples, the primary consideration is the probability of 'success'. This is usually followed closely by the financial costs. Success can be defined in many ways but for a couple, this almost universally means taking home a healthy baby (for some, the actual process of trying to achieve a pregnancy together is the focus).
A critical concept is the 'pregnancy rate'. Obtaining a pregnancy is never guaranteed with any approach (this includes intercourse, insemination or IVF) but for most couples the more attempts at conception they have, the more likely they are to conceive. For example, the rate of conception with intercourse (and similarly for insemination) is relatively low - for most couples it amounts to about 20% per cycle when a cycle is defined as a month and there are no major barriers to conception (such as advanced female reproductiveage). However, over the course of many attempts the cumulative chance of conception becomes very high - about 80% over the course of one year. Conversly, IVF has a very high chance of success per cycle - in the range of 50% for most couples. Obviously there is a huge difference in cost between having intercourse and undergoing IVF. Because these differences are so large, the financial expense and time required for each attempt at conception becomes an important consideration - and sometimes is the deciding factor.
For the approach of sperm retrieval and IVF, the probability of a pregnancy almost entirely depends on female fertility - obtaining sperm from the man is rarely an issue nor is their quality generally a problem. By far the most important female factor is age. There are multiple other considerations including estimates of ovarian reserve (inherently imprecise), reproductive health (for example, uterine anatomy), general health (for example, women with high body mass index may be precluded from hyperstimulation/IVF) and prior pregnancy history.
Determing the chance of a pregnancy following a vasectomy reversal is much more complicated since in addition to all the female factors mentioned above one must also consider the chances of a successful reversal. Furthermore, it may take several months to determine if the reversal has been successful (or has failed) and of course natural conception has a lower per cycle succcess rate than IVF. In some cases, the time required to determine if the VR has been successful is unacceptable - especially when advanced female reproductive age is a consideration.
In some cases, obtaining an individualized assessment of the chances of success is necessary. For an estimate of the success of IVF/ICSI a referral to a fertility clinic can be made. This will almost always require some testing to evaluate female fertility.
Success Following Vasectomy
Success following a vasectomy can be defined in 3 ways:
Technical success: return of any sperm to the ejaculate. This is the most commonly used and easily assessed measure but it can be significantly misleading (see below)
Good technical succss: Return of high numbers of sperm to the ejaculate - greater than 10 million/mL. At this concentration, there is at the very least a good chance of obtaining a pregnancy (if there are no significant female factors) and insemination (IUI) also becomes an option.
Pregnancy
The key to at least having a chance of pregnancy is to have a good technical result. In the absence of high numbers of sperm, the chances of a pregnancy are substantially reduced. The absence of a good technical result, oftentimes in conjuction with female factor, is the primary reason for the failure of VR to result in a pregnancy. Note that unlike IVF, the per cycle success rate, when defined as the probabiliy of pregnancy during any month, is the same as for natural conception when a good technical result is achieved. Just as per natural conception, the cumulative chance of pregnancy will substantially increase over time with more attempts.
THE CHANCE OF A SUCCESSFUL VASECTOMY REVERSAL IS PRIMARILY DEPENDENT ON THE LENGTH OF TIME THE VAS DEFERENS HAS BEEN OBSTRUCTED (THE 'OBSTRUCTIVE INTERVAL').
Shorter invtervals are associated with a high chance of success and longer intervals a lower chance. There is no 'magic cutoff time' beyond which reversal is guaranteed to fail (or conversely guaranteed to succeed). Rather, the chances of success gradually diminish over time. Most men with an obstructive interval of a few years will have a successful procedure whereas very few with obstruction greater than 15 years will succeed. As always, there are going to be exceptions.
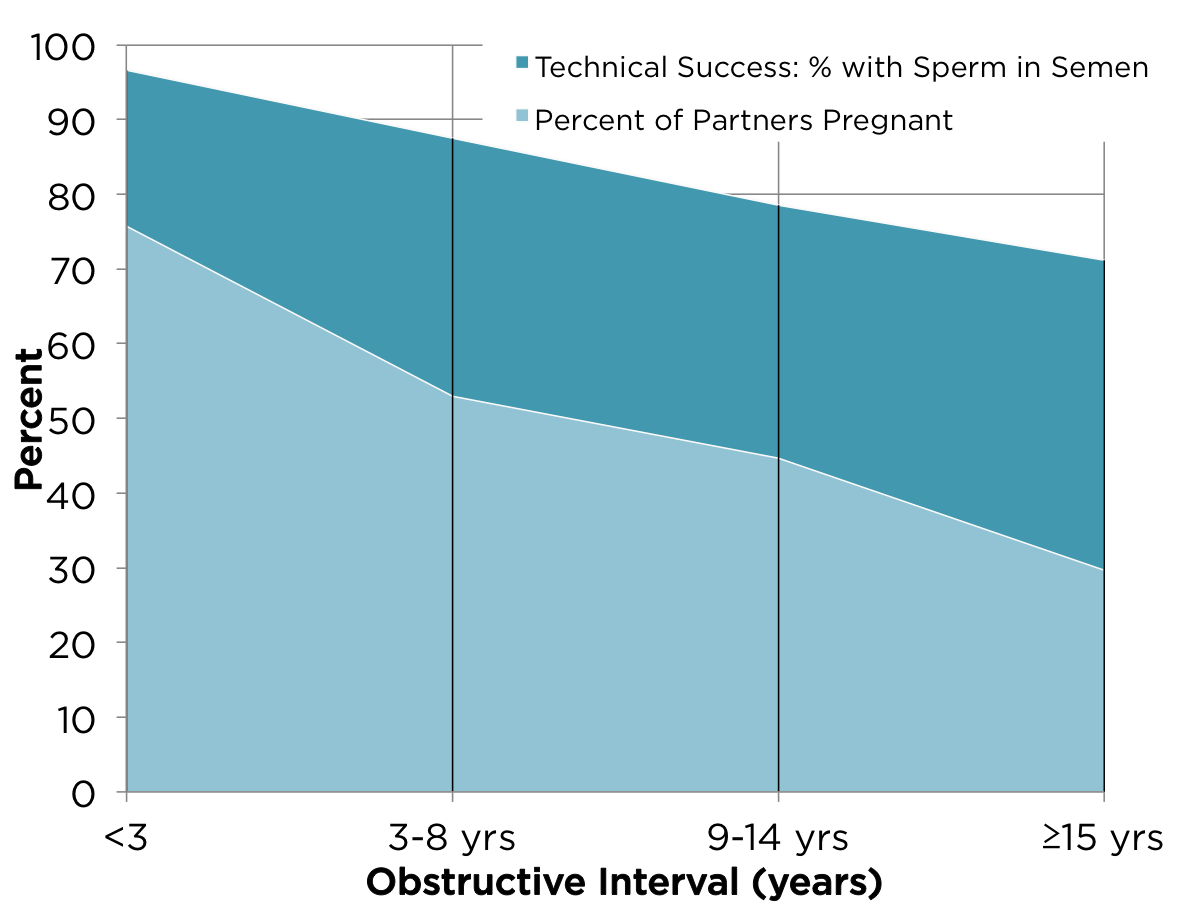
Success was defined in 3 ways (see above). The chances of technical success diminish over time. What is not well appreciated is that the chances of a good technical success diminish at a faster rate. Furthermore, the chances of a pregnancy will diminish even more rapidly over time. Note that many studies and surgeons will note the chances of technical success without considering the chances of pregnancy (see the graph below which is probably the most quoted study on technical success following vasectomy reversal.
There are a number of reasons for the more rapid fall-off in the chances of pregnancy compared to technical success as the obstructive interval increases.
The chances of a good technical success decrease faster then for technical success. The chances of requiring a vasoepididymostomy (a more complex and ultimately less successful approach than vasovasostomy increase over time. There is more likelihood of upstream obstruction as well. The quality of the fluid at the time of vasectomy help determine the approach.
There is a tendency for there to be female factors at play with prolonged obstructive intervals - especially age. A man who is considering a reversal after 15 years is more likely to have a spouse who is young but from a reproductive standpoint not at an age where the highest chances of natural conception occur (this is any woman less than 25-30 years of age).
Obviously surgeon skill and experience make a large difference. Specialized training in vaso-epididymostomy and coordination with an infertility centre are pre-requisites to obtaining a good result. We have the ability to cryopreserve your sperm and the additional training and experience required to perform a vasoepididymostomy.
Figure: Technical success and pregnancy decrease with the time from vasectomy. From the Vasovasostomy study group.
The above numbers are the most frequently quoted results for vasectomy reversal but are overly optimistic in many circumstances. This study lost multiple patients to follow-up and did not account for that loss in reporting the results. It is estimated that instead of an average technical success rate of 90-95% that a more realistic outcome is 80-85%. Furthermore, the chances of a good technical results are going to be lower. What one needs is an individual assessment in order to make an informed decision.
There are many reasons why sperm may not return to the ejaculate following vasectomy including upstream obstruction, scarring at the site of the anastomosis and decreased sperm production. Ultimately, some men are going to have their vasectomy reversal fail. When can failure be declared? It takes up to 2 years - this is an important consideration if expediency is the most important factor (e.g. advanced female reproductive age). Here is some guidance on timelines for return of sperm to the ejaculate (important: success rates are quoted for men with obstructive intervals less than 8 years and who are candidates for vasovasostomy):
Months 3-6: 3/4 of men have return of sperm
Months 6-12: 1/2 of remaining men have return of sperm
Months 12-18: 1/4 of remaining men have return of sperm
One can see that the rate of success diminishes over time but that ultimately some men require many months to determine if the surgery has been successful (or conversely, has failed). There have been cases where sperm may not appear for 2-3 years after reversal, but they are rare.
For couples in whom men have a reasonable chance of a good technical result and in whom there are no substantial female factors, vasectomy reversal is often the treatment of choice. Vasectomy reversal may not be the best choice when the chances of a good technical result are low or where there is no 'luxury of time'. In couples in whom there is a substantial female factor, achieving a pregnancy is can be challenging no matter what option is selected - vasectomy reversal or sperm retrieval + IVF.
If vasectomy reversal fails, the options are to proceed with sperm retrieval (if one chose not to bank sperm at with testicular sperm extraction at the time of the vasectomy reversal) or an attempt at repeating the vasectomy reversal.
There is no one 'best' choice. Every couple must decide on their own which approach fits them best.
What is involved in vasectomy reversal?
The goals of vasectomy reversal are to achieve return of sperm to the ejaculate and insure against failure of the vasectomy by cryopreserving sperm at the same time. Not all reversals are successful and eliminating the chance of requiring another surgical retrieval by perserving sperm at the time of reversal is recommended in all men. Therefore, a vasectomy reversal is really a combination of procedures rather than one procedure.
Vasovasostomy: reconnecting the two cut ends of the vas deferens
Vasoepididymostomy: connecting the abdominal (distal) end of the vas deferens to an epididymal tubule
Sperm retrieval and cryopreservation, usually directly from the testis.
The highest success rates for vasectomy reversal occur with vasovasostomy UNLESS there is upstream obstruction, in the epididymis, for example. The quality of the fluid in the testicular (proximal) end of the vas deferens at the time of reversal is key. If there is a concern regarding the quality of the fluid, then the epididymis can be inspected to get a sense if there is scarring and vasoepididymostomy performed if indicated.
The procedure usually takes between 45-60 minutes per side through small incisions in the scrotum. Because the sutures which are used to sew the ends together are much smaller than a human hair, an operating microscope and specialized instruments are necessary. It is very important that there is no movement during the procedure and therefore vasectomy reversal is usually performed under a general anesthetic
Cost
Vasectomy reversal is not covered by the Medical Services Plan. The cost of the procedure pay for the use of a private operating facility including the nursing staff, equipment, disposables (e.g. sutures), the professional fees for the anesthesiologist and the surgeon. Please contact us for a quote.
Preparation
You must FAST before the procedure because it is done under a general anesthetic. This means nothing to eat or drink from midnight on prior to your procedure.
Please make arrangements for someone you know to accompany you home. By law, you cannot drive for 24 hours after surgery.
Stop any blood thinners or antiplatelet agents (such as coumadin/warfarin, aspirn or Plavix)
Shave your scrotum prior to coming in.
Bring an athletic support
After Procedure
If you have questions that are not answered here, please contact us.
What to Expect
It will be normal for you to have some pain and bruising following your procedure (though many men will have no bruising).
Cautions
If you have significant scrotal swelling please contact us as you may be developing a hematoma. Some minor bruising is normal.
Diet
There are no dietary restrictions.
Activity
Avoid vigorous physical activity and intercourse for about 5 days after your procedure as it can produce post-operative bleeding. You may bathe any time after the procedure.
Medications
You may resume all of your regular medications after your vasectomy reversal. If you are on blood thinners, you urologist will give you specific instructions but, in general, antiplatelets and anticoagulants (e.g. aspirin, plavix and coumadin/warfarin) should be discontinued about 7 days before surgery and can be resumed 7 days after the procedure.
Follow-up
We will contact you for follow-up. You may resume having intercourse about 2-3 weeks after the procedure. You will receive a laboratory requisition to check your semen analysis every 1-2 months for return of sperm until your partner is pregnant.